SUDDEN ONSET DEAFNESS IN AN ADULT
By Dr Parey Mohd Farooq
Sudden onset deafness, also known as sudden sensorineural hearing loss (SSNHL), is a condition in which an individual experiences a rapid loss of hearing in one or both ears. It can occur at any age, but it is most commonly seen in adults between the ages of 30 and 60. SUDDEN ONSET DEAFNESS IN AN ADULT
SSNHL affects approximately 5-20 people per 100,000 each year, with a higher incidence rate in men than in women. The exact cause of SSNHL is not yet fully understood, but it is believed to be a result of a viral infection, immune system disorders, or vascular disorders.
Symptoms of SSNHL can include a sudden loss of hearing in one or both ears, a feeling of fullness or pressure in the ear, tinnitus (ringing in the ear), and dizziness or vertigo. If you experience any of these symptoms, it is important to seek medical attention immediately.
Diagnosis of SSNHL typically involves a physical examination of the ear and hearing tests, such as an audiogram or a tympanometry test. In some cases, imaging tests such as an MRI or CT scan may also be necessary.
Treatment for SSNHL often involves the use of steroids, either orally or through injection into the ear, to reduce inflammation and promote healing. The success of treatment depends on the severity and underlying cause of the condition, with some cases showing partial or complete recovery of hearing, while others may result in permanent hearing loss.
Sudden onset deafness is a serious condition that requires prompt medical attention. If you experience any symptoms of SSNHL, it is important to seek medical care immediately. Early diagnosis and treatment can improve your chances of a successful recovery and help prevent permanent hearing loss.
Case Study
A 52 year Gentleman presented to his physician with bilateral otalgia, and tinnitus associated with subjective fever without any ear discharge. This was preceded by flu-like symptoms which had resolved two days prior to the current presentation, He was started on oral antibiotics with a clinical impression of Acute otitis media
However, two days later he developed unilateral hearing loss and vertigo, He seek advice from his General practitioner who referred him to the emergency department for Labyrinthitis. He was triaged in Ed and found to have facial palsy and labelled as Bell’s palsy for evaluation by the emergency physician.
Chief Complaints
Hearing loss of the right ear, Vertigo, and facial weakness.
Past medical history -Hypertension not complying with treatment, Heavy smoker
Vital signs: Pulse =78. BP=137/94. T=37.3. Spo2=98% on room air
Physical exam- Conscious, alert., GCS =15/15. , No motor or sensory deficit
HINTS exam =Head impulse test no catch-up saccade, Nystagmus on primary gaze, bidirectional with a torsional component. Vertical skew,
Sensorineural deafness on the right side with positive right-side cerebellar signs,
There was a lower motor neuron type of facial palsy on the right side.
Ipsilateral Miosis, ptosis and anhidrosis noted,
Rest of the systemic exam was unremarkable
Lab results revealed leukocytosis – 15.2 predominantly neutrophils, CRP=85
Lipid profile revealed elevated cholesterol and triglycerides.
Coagulation profile, Renal & liver function tests, and electrolytes. were within normal range.
CT head was reported unremarkable by the radiologist on duty
The stroke team evaluated the patient and was of the opinion that it’s most likely a complicated otitis media with Labyrinthitis.
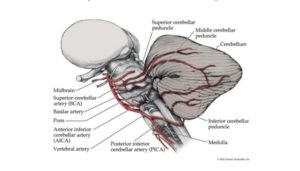
Ramsay hunt syndrome was also suspected, It was advised to refer the patient to ENT for evaluation. However, the Emergency physician was not convinced by the decision of the stroke team so escalated it to a neurology consultant on call & both came to the conclusion that it was a classical presentation of Anterior inferior cerebellar territory infarction.
The patient was admitted under neurology and the subsequent MRI on the next day reported cerebellar infarction in the territory of AICA.
The patient was started on antiplatelet therapy and statins, His ataxia resolved, facial palsy improved but continued to have unilateral deafness
Teaching message: Acute unilateral deafness shouldn’t be labelled as idiopathic and should always be evaluated thoroughly, especially in people with a risk of atherosclerosis
–Non-contrast head CT shouldn’t be used to rule out any brain infarction.
-Whenever and wherever there is a clinical suspicion,the patient should be admitted for subsequent MRI accordingly
The author is MD, MRCEM, Member of the European Society of Emergency Medicine, Emergency medicine specialist at the University Hospital Of Morecambe Bay NHS Trust, Lancaster United Kingdom


Comments are closed.